How I Found My Way Back: A Real Talk on Postpartum Healing
After giving birth, I felt lost—like my body and mind no longer belonged to me. Many women face the same struggle, yet we rarely talk about it openly. Postpartum recovery isn’t just physical; it’s emotional, mental, and deeply personal. This journey taught me how to reclaim my health with patience, self-awareness, and small, sustainable changes that truly worked. I didn’t need drastic measures or perfect routines—just honest, science-backed choices that honored my body’s needs. What I discovered wasn’t a quick fix, but a lasting shift in how I care for myself. This is a conversation long overdue, one that every woman deserves to hear.
The Hidden Battle: Understanding Postpartum Recovery
Postpartum recovery extends far beyond the physical healing of childbirth. It encompasses a complex web of emotional shifts, hormonal fluctuations, sleep disruption, and a profound adjustment to a new identity. For many women, the weeks and months after delivery are marked not by celebration, but by exhaustion, confusion, and a sense of disconnection from their former selves. The reality is that the body undergoes massive physiological changes during pregnancy and delivery, and it requires time—often much more than society acknowledges—to restore balance. Yet, cultural narratives often promote the idea of a rapid “bounce back,” pressuring women to return to pre-pregnancy weight and activity levels within weeks. This expectation is not only unrealistic but can be harmful, leading to increased stress, shame, and delayed healing.
Common misconceptions about postpartum recovery include the belief that rest alone is sufficient, that mood changes are just “baby blues” and will pass quickly, or that physical symptoms like incontinence or pelvic discomfort are normal and should be accepted. While some degree of fatigue and emotional sensitivity is expected, persistent symptoms may indicate underlying issues that require attention. Research suggests that up to 80% of new mothers experience some form of mood disturbance in the first weeks after birth, and approximately 1 in 7 will develop postpartum depression. Additionally, studies show that around half of women report ongoing physical symptoms such as diastasis recti, pelvic floor dysfunction, or low energy levels beyond the six-week postpartum checkup. These statistics underscore the need for a more comprehensive, individualized approach to recovery.
Another critical aspect of postpartum healing is recognizing that it is not a linear process. Progress may come in waves—some days feel manageable, while others bring setbacks. One woman may regain strength quickly, while another may need months to feel like herself again. This variation is normal and should be respected. The timeline for recovery depends on numerous factors, including the type of delivery, pre-existing health conditions, support systems, and mental well-being. By shifting the focus from speed to sustainability, women can begin to view recovery as a journey of reconnection rather than a race to return to “normal.” Acknowledging this complexity is the first step toward building a healthier, more compassionate postpartum experience.
Listening to Your Body: The First Step in Health Management
One of the most powerful tools in postpartum healing is learning to listen to your body. After childbirth, the body sends subtle—and sometimes not-so-subtle—signals about its needs. These cues include fatigue, pain, emotional shifts, and changes in appetite or sleep patterns. However, in the early weeks of motherhood, these signals are often ignored or overridden due to the demands of caring for a newborn. Women may push through exhaustion, dismiss pelvic discomfort, or minimize feelings of sadness, believing they must “tough it out.” This pattern of suppression can delay healing and increase the risk of long-term complications such as chronic fatigue, pelvic floor disorders, or mood disorders.
Developing self-awareness begins with simple daily check-ins. Taking a few moments each morning and evening to assess energy levels, mood, and physical sensations can provide valuable insight into overall well-being. For example, noticing persistent low energy despite adequate sleep may indicate nutritional deficiencies or underlying hormonal imbalances. Tracking mood fluctuations over time can help identify patterns and determine whether emotional changes are part of normal adjustment or signs of a more serious condition. Sleep quality is another key indicator—frequent nighttime awakenings, difficulty falling back asleep, or unrefreshing sleep can all impact recovery. These observations do not need to be recorded in detail; even a brief mental note can foster greater attunement to the body’s needs.
Practical strategies for tuning into bodily signals include pausing before reacting to demands, asking “What do I need right now?” and allowing space for rest without guilt. Mindful breathing, gentle stretching, or sitting quietly with a cup of tea can create moments of presence that enhance body awareness. It’s important to approach these check-ins without judgment—there is no “right” or “wrong” way to feel during recovery. The goal is not to fix everything at once but to cultivate a relationship of trust and care with the body. When women honor their physical and emotional signals, they lay the foundation for sustainable healing and long-term well-being.
Rest Reimagined: Rethinking Recovery in Real Life
The concept of rest is often oversimplified in postpartum conversations, particularly with the common advice to “sleep when the baby sleeps.” While well-intentioned, this guidance can feel unattainable or even frustrating for many new mothers. Sleep is just one form of rest, and for those struggling with insomnia, anxiety, or fragmented sleep, waiting for the perfect opportunity to rest may lead to prolonged exhaustion. True recovery requires a broader understanding of rest—one that includes mental, emotional, and physical relaxation, even in small doses. Reimagining rest means recognizing that healing can happen in moments of stillness, connection, and reduced stimulation, not just during sleep.
Alternative forms of rest include seated relaxation with eyes closed, listening to calming music, practicing mindful breathing, or engaging in quiet conversation with a trusted friend. These activities may seem minor, but they allow the nervous system to shift from a state of constant alertness to one of calm and repair. Delegating tasks is another essential component of rest. Asking for help with household chores, meal preparation, or childcare—even for short periods—creates space for recovery. Partners, family members, or friends can assist with simple duties like folding laundry, running errands, or holding the baby while the mother rests. When support is limited, identifying small ways to reduce demands—such as using disposable dishes or simplifying routines—can make a meaningful difference.
Creating micro-moments of recovery throughout the day is both practical and effective. For example, placing a pillow under the arms while feeding can reduce shoulder strain. Sitting in a comfortable chair with feet elevated during feeding sessions promotes circulation and relaxation. Even a two-minute pause to take deep breaths between tasks can reset the nervous system. These small acts accumulate over time, contributing to improved hormone regulation, reduced inflammation, and enhanced tissue repair. Quality rest supports the body’s natural healing processes, including the regulation of cortisol and the restoration of depleted energy reserves. By redefining rest as an active, intentional practice rather than a passive state, women can integrate healing into the realities of new motherhood.
Movement That Makes Sense: Gentle Reconnection with Your Body
Reintroducing movement after childbirth should be approached with care and patience. The body has undergone significant structural and hormonal changes, and rushing into intense exercise can lead to injury, pelvic floor dysfunction, or prolonged recovery. Instead, gentle, progressive movement helps rebuild strength, improve circulation, and support mental well-being. The focus should not be on burning calories or losing weight, but on reestablishing a positive connection with the body. Walking is one of the safest and most effective forms of early postpartum activity. Starting with short, slow walks around the neighborhood—even five to ten minutes—can boost mood, enhance blood flow, and support core and pelvic floor recovery.
Pelvic floor awareness is a critical component of postpartum movement. During pregnancy and delivery, these muscles are stretched and weakened, which can lead to issues such as incontinence or pelvic organ prolapse. Gentle pelvic tilts, diaphragmatic breathing, and kegel exercises (when appropriate) help retrain these muscles. However, it’s important to perform these exercises correctly—pulling the pelvic floor upward and inward without holding the breath or tightening the glutes. A healthcare provider or pelvic floor physical therapist can offer personalized guidance. Gentle stretching, particularly of the hips, lower back, and shoulders, also supports recovery by releasing tension accumulated during pregnancy and childbirth.
A sample weekly progression plan might begin in the first week with seated breathing exercises and short walks. By weeks two to four, women can gradually increase walking duration to 15–20 minutes and add gentle stretching. Around six weeks postpartum—after receiving medical clearance—light bodyweight exercises such as modified squats or wall push-ups can be introduced. Core engagement should be approached cautiously, avoiding traditional crunches or planks until the abdominal muscles have sufficiently healed. Movements should always be pain-free and performed with attention to alignment and breath. Over time, increased activity supports not only physical recovery but also emotional resilience by reducing stress hormones and increasing endorphins. The key is consistency over intensity, honoring the body’s pace rather than pushing beyond its limits.
Fueling Healing: Nutrition Without the Hype
Nutrition plays a vital role in postpartum recovery, yet it is often overshadowed by fad diets and unrealistic expectations. The postpartum body needs sustained energy, essential nutrients, and hydration to support healing, milk production (if breastfeeding), and daily functioning. Rather than focusing on restriction or rapid weight loss, the goal should be balanced, nourishing eating habits that are realistic for a tired, time-pressed new parent. Key nutrients include iron, which helps replenish blood loss; protein, which supports tissue repair; fiber, which aids digestion; and healthy fats, which contribute to hormone regulation and brain health. These can be obtained through whole, accessible foods such as lean meats, eggs, legumes, whole grains, vegetables, fruits, nuts, and seeds.
Realistic meal ideas include oatmeal with banana and peanut butter for breakfast, lentil soup with whole grain bread for lunch, and grilled salmon with roasted sweet potatoes and steamed broccoli for dinner. Snacks such as yogurt with berries, apple slices with almond butter, or hard-boiled eggs provide quick energy and sustained fullness. Hydration is equally important—breastfeeding women may need up to 16 cups of fluid per day, though individual needs vary. Keeping a large water bottle nearby and sipping throughout the day can help meet this demand. Herbal teas, broths, and milk are also good options, but sugary drinks and excessive caffeine should be limited.
It’s crucial to avoid restrictive diets and extreme cleanses during early recovery. These approaches can deplete energy, impair milk supply, and increase the risk of nutrient deficiencies. The body needs calories and nutrients to heal, and deprivation only prolongs fatigue and emotional strain. Instead of aiming for perfection, women should focus on progress—eating regularly, including a variety of food groups, and being kind to themselves when meals are less than ideal. Meal prepping on higher-energy days, accepting food gifts from friends, or using simple frozen or canned ingredients can reduce daily stress. By prioritizing nourishment over aesthetics, women support their long-term health and set a positive example for their families.
Emotional Anchors: Managing Mental Well-being in Transition
Emotional well-being is an integral part of postpartum recovery, yet it is often the most overlooked. The transition to motherhood brings profound changes in identity, routine, and relationships, which can lead to mood fluctuations, anxiety, and feelings of isolation. It is completely normal to feel overwhelmed, tearful, or uncertain in the early weeks. These emotions are not signs of weakness but natural responses to a life-altering experience. However, when mood disturbances persist beyond two weeks, interfere with daily functioning, or include thoughts of harm to oneself or the baby, professional support should be sought. Conditions such as postpartum depression, anxiety, or obsessive-compulsive disorder are treatable, and early intervention improves outcomes.
Evidence-based coping tools can help manage emotional challenges. Journaling, even for a few minutes a day, provides a safe space to express thoughts and track mood patterns. Brief mindfulness practices—such as focusing on the breath for one minute or noticing sensory details during feeding—can reduce anxiety and increase presence. Connecting with other mothers, whether through in-person groups or online communities, offers validation and reduces feelings of loneliness. Sharing experiences, asking questions, and realizing “I’m not alone” can be deeply comforting. Partners and family members can also play a supportive role by listening without judgment, offering reassurance, and encouraging self-care.
It’s important to differentiate between normal adjustment and signs that professional help is needed. Mild mood swings, fatigue, and occasional sadness are common. However, persistent sadness, inability to bond with the baby, extreme worry, or loss of interest in activities may indicate a more serious condition. Seeking help from a healthcare provider, therapist, or counselor is a courageous and necessary step. Therapy, support groups, and, when appropriate, medication can make a significant difference. Women should know that asking for help is not a failure—it is an act of strength and self-responsibility. By normalizing conversations about mental health, we create a culture where healing is possible for everyone.
Building a Personalized Plan: From Survival to Thriving
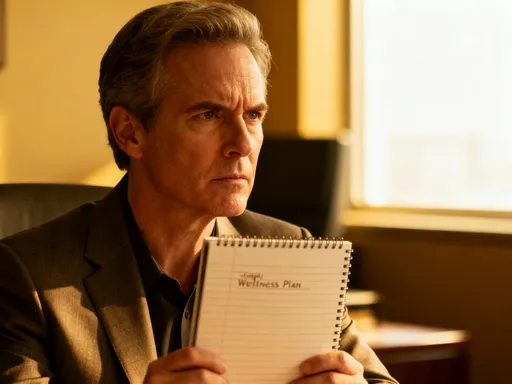
Every woman’s postpartum journey is unique, and a one-size-fits-all approach does not work. The key to sustainable recovery lies in creating a personalized health management plan that reflects individual needs, resources, and pace. This plan should integrate the principles discussed—listening to the body, redefining rest, gentle movement, balanced nutrition, and emotional support—into a flexible routine. Start by setting small, achievable goals, such as drinking more water each day, taking three short walks per week, or journaling twice a week. Track progress in a simple way, such as marking a calendar or using a notes app, without pressure to be perfect. Celebrate small wins, knowing that consistency matters more than intensity.
Involving partners or caregivers in the recovery process can enhance success. They can assist with practical tasks, provide emotional support, or simply remind the mother to pause and rest. Open communication about needs and boundaries helps build a supportive environment. For example, a partner might take over nighttime feedings if bottle-feeding, or handle bedtime routines to allow uninterrupted rest. Family members can contribute by preparing meals, doing laundry, or watching the baby for short breaks. Even small acts of support can significantly reduce stress and create space for healing.
The ultimate goal is not to return to who you were before childbirth, but to evolve into who you are now—with greater resilience, awareness, and compassion. Postpartum recovery is not about perfection; it’s about progress, patience, and presence. It’s about learning to care for yourself as deeply as you care for your child. By rejecting unrealistic expectations and embracing a holistic, evidence-based approach, women can rebuild strength, balance, and confidence. This journey is not a detour—it is an essential part of becoming a mother. Always consult a healthcare provider before starting any new health practice, and remember: healing is not a race. It is a promise you make to yourself—one small, intentional step at a time.